Long-Post-Short-Good. It doesn’t take long to become immersed in the ebbs and flows of the call schedule. On Long Days, the medical team admits patients from noon through the evening — each one requiring detailed history, a thorough physical exam, a working diagnosis, and orders for the appropriate nursing care, diagnostic testing, and medications. On Good Days, there are no new patients. Instead, we care for those patients that remain in the hospital and discharge those that are healthy enough to go. We leave early in the afternoon to recharge before the cycle begins again.
That Wednesday was a Good Day. Our patients were doing well, and several would be discharged from the hospital. On my own, student-sized list, I had three stable patients. Freed from preparing meticulous presentations or writing exhaustive admission notes, I planned to accompany one of our most familiar patients to his procedure.
Mr. P was a man in his seventies who had been on my list for nearly a week. He was low maintenance: each morning, he would tell me that he’d slept well the night before and that he’d had no symptoms, and that his only complaint was that the hospital food didn’t compare to his home cooking. Our daily routine closed with Mr. P’s lavishing praise on everybody involved in his care — “From the janitor up to the doc-in-charge, you all are second to none,” and awkward acceptance of it — “There’re a lot of good people here.”
This ritual was briefly interrupted when Mr. P attended his father’s funeral. After deciding that he could safely leave for several hours, we arranged for him to be swiftly readmitted when he returned later that night. All went smoothly, and his gratitude for this basic accommodation became a new part of his daily effusions.
In fact, he had never had any symptoms, save for some mild difficulty breathing when he attempted to climb, in his words, “multiple sets” of stairs. He was only here because, at a routine check-up, his primary care doctor noted that his heart was beating 160 times per minute, far enough above normal to warrant evaluation in the Emergency Department. Despite his denial of symptoms, an ultrasound showed that his heart was not efficiently pumping blood. He was in heart failure, and the cardiologists suspected that his fast heartbeat may have been the cause. Our job was to find the proper medications and doses to slow his heart rate into an acceptable range.
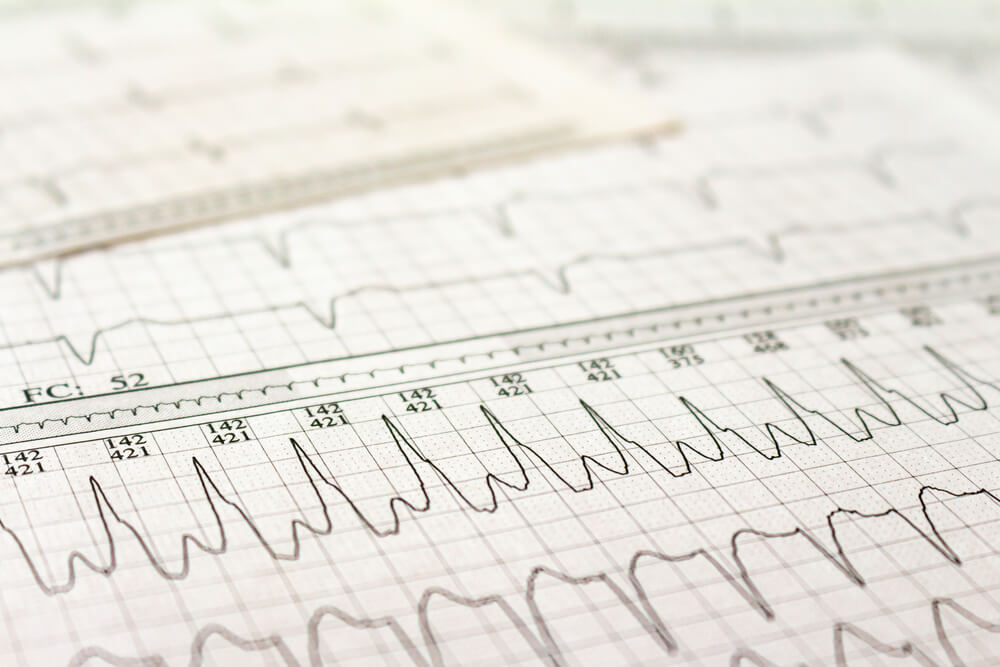
Eventually, we were able to control Mr. P’s heart rate with a medication. But it remained in an abnormal, and potentially dangerous, rhythm. The cardiologist recommended another approach — electrical cardioversion. In this procedure, wires connected to a machine called a defibrillator/cardioverter are attached to the patient’s chest. The machine delivers a shock at a precise point during the heart’s cycle to reset the electrical pathways. It’s used frequently in patients with arrhythmias that are either causing dangerously low blood pressure or aren’t resolving with medications, like Mr. P’s. This procedure immediately corrects the arrhythmia about 90 percent of the time, although the results are often not permanent. The sudden change in rhythm may cause blood clots to break free from the heart and enter the brain, causing a stroke.
That Wednesday morning, I went to the anesthesia recovery unit, where the procedure would take place. I introduced myself to the cardiologist, and he began to explain the procedure to me. He walked me through the information contained in the electrocardiographic tracing of Mr. P’s heart on the monitor next to his bed. As we talked, the anesthesiologist sedated Mr. P and another cardiologist ran a long ultrasound probe down Mr. P’s esophagus to check for any clots in the chambers of the heart. The first cardiologist reviewed the anatomy of Mr. P’s heart on the ultrasound for me as technicians applied the wires to his chest. The ultrasound was clear; it was time to proceed with the cardioversion.
I stood with the cardiologist next to the defibrillator/cardioverter as he synchronized the machine to the patient’s heartbeat. He pressed the CHARGE button, and the machine sounded a monotonous “beep” as it generated the voltage to correct Mr. P’s arrhythmia. The light surrounding the SHOCK button turned red and the beep stopped. “Clear the patient,” the cardiologist said. The anesthesiologist removed his hands from Mr. P and stepped back.
“The patient’s clear,” he responded.
The cardiologist turned to me: “Why don’t you push the button. Make sure to hold it down until the light goes on.”
“Sure,” I replied, slightly surprised but pleased that my engagement with his teaching warranted a small reward. I placed my thumb on the button and pressed down. The SHOCK light went dark. I kept holding. A second “beep” sounded, and the light turned back on. I looked at Mr. P, expecting to see some sign that his heart was back in its normal rhythm. I did not see that the line on the monitor, which had just shown the irregular beating of Mr. P’s heart, had gone flat.
Asystole is the complete loss of electrical activity in the heart — it is the absence of rhythm. For each moment that the heart is not pumping blood, vital organs such as the brain and kidneys start to die. Deprived of oxygen, tissues start to produce lactic acid, which causes further damage as it accumulates. In cardiopulmonary resuscitation (CPR), chest compressions slow this process by circulating the blood, while rescue breaths exchange fresh oxygen for toxic carbon dioxide in the lungs. In-hospital CPR restores a patient’s circulation 40 percent of the time. However, only about 15 percent of these patients ultimately leave the hospital alive.
Before I had realized that Mr. P’s heart had stopped, I saw the cardiologist start chest compressions. Several nurses descended on Mr. P’s bed. The anesthesiologist took charge, assigning roles and requesting medications. I was not assigned a role, so I stepped to the edge of the scene. I looked at the monitors that showed Mr. P’s missing heartbeat, but my mind was elsewhere. All I could think about was that I had pressed the button that stopped this patient’s – my patient’s — heart.
Fortunately, Mr. P’s heart started beating again after only 90 seconds of CPR, but it was beating too slowly to deliver sufficient blood to his organs. He was part of the 40 percent, but he needed more help to make it to the 15 percent. The cardiologist started to pace his heart through his skin with the wires already stuck to his chest. He then inserted a wire through the jugular vein in Mr. P’s neck to control his heart rate more stably. The anesthesiologist had placed a breathing tube down Mr. P’s throat, which he connected to a ventilator to help Mr. P breathe. Gradually, I sensed growing optimism about his survival.
Eventually, he was stable enough to move to the Intensive Care Unit. I must have waited a moment too long to leave the scene after Mr. P was wheeled away. One of the cardiologists came up to me and patted me on the back. “That wasn’t your fault, just so you know.” I knew this already — I had followed the cardiologist’s instruction exactly, and all I did was press a button on a machine intentionally designed to be foolproof in high-stress situations. But his reassurance made me feel better, knowing that somebody in the room had seen me, standing at the periphery and grappling with the enormous power of medicine as I watched the nurses and doctors bring Mr. P back to life. He left, and I went upstairs to update my team on what had just happened.
Two days later, Mr. P was out of the ICU and back in his old room. He looked a little more tired than before, and he had a large gauze dressing on his neck where the pacing wire had passed through his skin. I asked him if he remembered anything from that Wednesday morning, and he said that he just remembered an intense, pounding pain on his chest — the chest compressions of CPR. He quickly returned to his familiar praise of the team, “from the janitors to the doc-in-charge.” I told him that he could go home later that day if he felt up to it, which seemed to move me more than him. “Of course,” he said, “the worst thing is, I made a whole chicken before I came in and divided it up for the week. I suppose I’ll just throw it out and start over again.”
That afternoon, I was returning to my computer with a fresh coffee, preparing to write notes, make calls, and read about the topics that had come up on our team’s morning rounds. I saw a man briskly approaching the elevators with the buoyancy of a jog. He was wearing orange leather cowboy boots, light blue jeans, a grey crew neck sweatshirt, and a huge smile underneath his cowboy hat. It was Mr. P.
He saw me coming and doffed his hat. “Thanks for everything, doc,” he said, and he entered the open elevator door.